
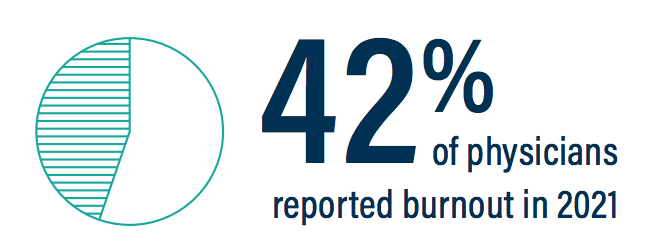
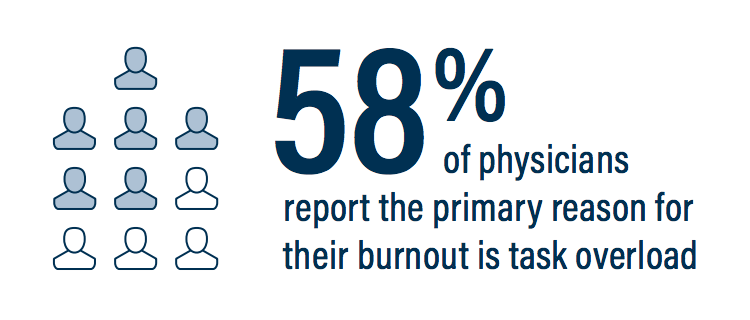
Chief Complaint: Physician Burnout
Physician burnout is a real issue. Overloading a physician’s daily tasks with administrative steps that could be assigned to other, more skilled data entry experts, has added fuel to the fire of EMR systems that just don’t fit the way they see their patients. We’re losing good physicians because they just don’t want to run in this rat race any longer.
Solution: ELTS alleviates physician burnout by providing simple dictation and sign-off workflows in a system that fits the way they see their patients.
Chief Complaint: Time-consuming process to document notes
Many providers find that the EMR has decreased efficiency and patient thru-put due to non user friendly workflows and difficult navigation. Quite often, physicians find that the EMR actually adds significant hours to their workday. It’s not uncommon that providers are in the office after hours completing their notes. Sometimes they have to finish them at home on the weekends. Proponents of EMR argue that electronic records streamline and reduce physician time spent with documentation, but nothing could be farther from the truth. many EMR systems are cumbersome and time-consuming, and EMR fatigue is a real issue for physicians.
Solution: Eagle’s Landing facilitates a return to dictation as a quicker, more accurate way to document within the EMR. No more endless clicks to produce a less-than report that really isn’t a wholly accurate account of the patient’s visit. The problem has been forcing busy physicians to change the way they see their patients to fit to the technology. ELTS feels this is backwards and contrary to efficiency. The key is in the workflow, and your workflow should be based upon the way you see your patients. ELTS workflows reclaim computer documentation time and direct it back to patient interaction, and after-hours documentation back to after-hours personal time.
Chief Complaint: Interruption of the doctor-patient relationship
We must take great care not to let the computer come between physicians and their patients. The art of medicine requires that doctors actually talk and listen to their patients. We must not forget the value of interacting with patients, looking them in the eye, and providing them undivided attention. Computers, laptops, and iPads in exam rooms foster distractions and often demand more of the doctor’s time than the patient receives. Doctors who make it a point to leave the laptop at the workstation and put notes in the EMR after the patient has exited the exam room are left finishing notes after hours. It’s no wonder that physicians and patients alike are quite frustrated. Patient dissatifaction runs high and patients express their discontent, not only to their care providers, but also on social media and in online practice reviews. The sacredness of the doctor-patient relationship has suffered greatly.
Solution: Through the use of simple workflows that are easy to use, ELTS improves the patient-physician relationship by re-claiming the physician’s time and directing it back to the patient.
Chief Complaint: Errors, lack of detail in Documentation
Most EMRs are plagued by erroneous data and lack of detail. Some errors and omissions are even libelous to the physician and/or the practice. Point and click and drop-down menu capabilities of most EMR systems introduce and even promote propagation of this erroneous data, and patients are wising up to errors in their medical records. Unless a physician takes the time to audit the electronic record on each visit, inaccurate information can be placed in a record and continued forward. Medication lists are three pages long and full of duplicate medications, all with slightly different dosages. Referring physicians find it impossible to figure out exactly what meds the patient takes and at what dose. Auto-populate and recall functions can lead to documentation of things that were never done, such as particular physical exam components like an ear exam for a GI preop visit.
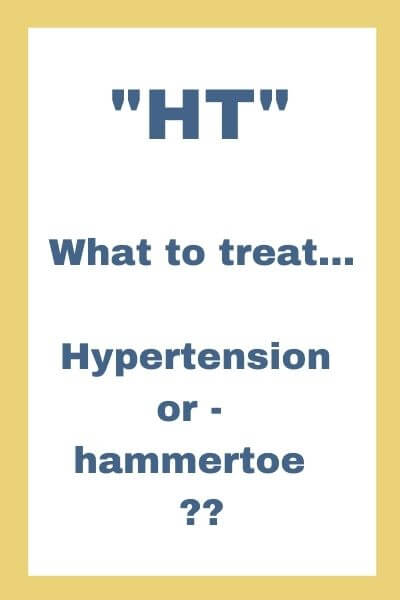
Errors of omission are real issues for the patient, especially when dealing with insurance authorizations and disability determinations. When there are chronic, progressive diagnoses, new notes from old notes, while perhaps a quick click, are disastrous for showing progression of disease. This unintended consequence creates its own additional set of steps for the physician by adding peer-to-peer phone calls, letters upon letters of explanation, and endless copying of notes and back-up documentation by the clinic staff. Simply capturing descriptive details of the patient’s disease progression, and not reducing completeness and accuracy to only the words and phrases that appear in a drop-down list, will eliminate many of these extra steps from an already full plate of daily physician tasks.
Solution: Dictation is the quickest, easiest, most effective way to accomplish this level of detail. Our patients deserve this kind of quality in their records and Eagle’s Landing helps you provide it.
EMR errors from actual patient notes
Auditor: Elisa Comer, ELTS Exec Dir, CPHIMS, CPEHR, CPHIT, CQA (used with permission)
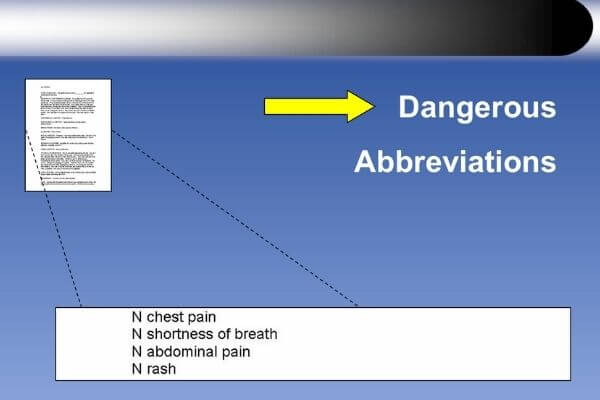
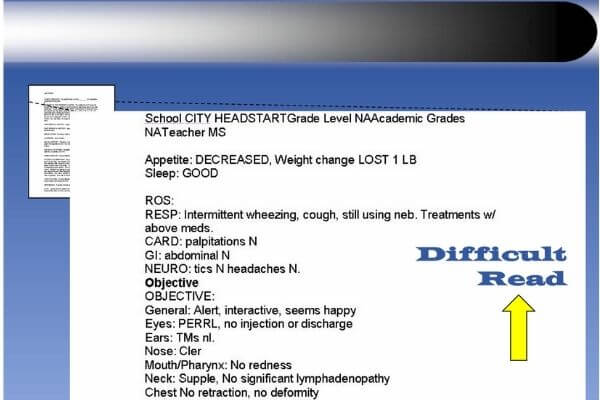
From fragmented formatting to non-standard, make-up-your-own abbreviations, EMR notes are often hard to decipher, which is interruptive to the patient visit and often to their care.
And for the record… does “N” mean “no” or “normal” – ??
and, why is “N” better than “No” – ??
???
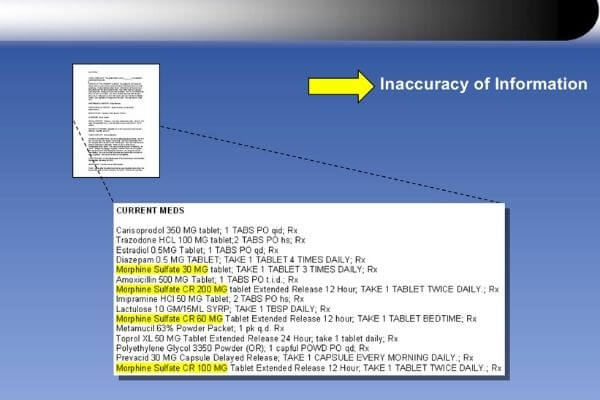
Confirm morphine dose – ??
Patient was postop and tapering to zero. Due to previous doses not being discontinued in the EMR system, pt was erroneously flagged for opioid abuse.
(Rx list generated by drop-downs)
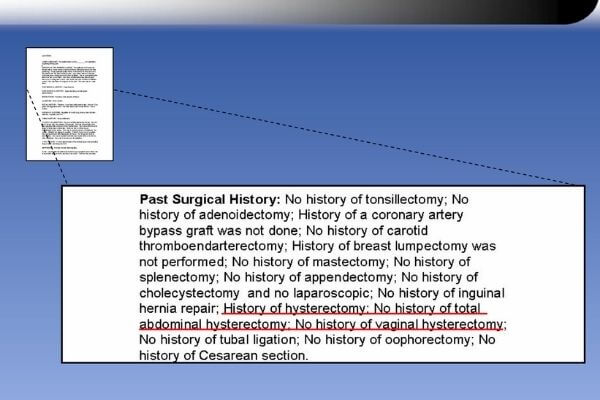
So, did this patient have a hysterectomy?
(Past Medical History generated by click-based charting, then auto-copied verbatim to new clinic visits x14 months)
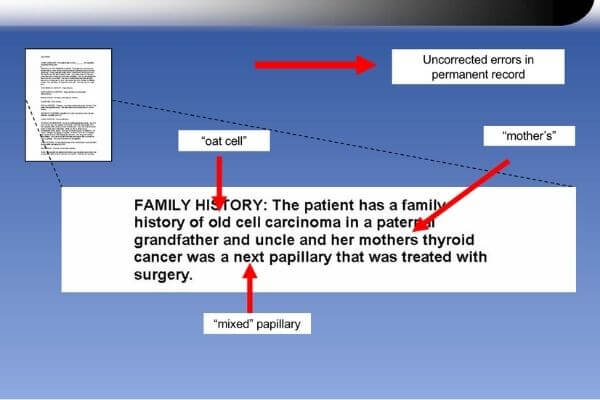
Inaccurate terms left in the patient’s permanent record.
MD response when audited, “Any doctor reading that will know what I meant.”
(Clinic-based speech recognition)
Chief Complaint: Cumbersome tasks for clinic staff

Carrying paper charts around becomes a thing of the past with the ELTS admin suite. Everything is digital, accessible online from desktop and smartphone, and there’s no need to print finished reports unless you just want to. Currently printing referral letters? No need to do that with our tools. You can maintain referring MD database and send letters right in the system.
Editing reports is done in seconds with the audio dictation attached to each note. No more chasing down a busy physician or waiting days to re-listen to voice files. Quick. Easy.
Bi-directional interfacing eliminates the need to print/scan/fax daily schedules, and the step of printing notes and scanning into the record is eliminated on the spot.
Solution: ELTS utilizes these steps and more as we build a workflow that eliminates cumbersome, time-consuming steps for your clinic staff. Office personnel report great satisfaction using our technology to process patient reports.